Complex Post-Traumatic Stress Disorder (C-PTSD) is a psychological condition that arises in response to prolonged, repeated trauma. While it shares some features with PTSD, it is a distinct disorder due to the severity and frequency of the traumatic experiences involved. Individuals suffering from C-PTSD often experience a variety of debilitating symptoms that affect their emotional, psychological, and social well-being. In this article, we will explore 17 key symptoms of C-PTSD, shedding light on the profound impact this disorder can have on one’s life.
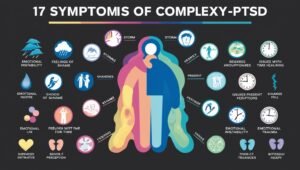
1. Emotional Dysregulation
One of the most prominent symptoms of C-PTSD is emotional dysregulation. Individuals with this disorder often find it difficult to manage their emotions, leading to extreme mood swings, irritability, and feelings of overwhelming sadness or anger. This inability to control emotions can disrupt personal relationships and make daily life more challenging.
2. Persistent Feelings of Shame and Guilt
Those suffering from C-PTSD often experience intense feelings of shame and guilt, even when these emotions are unwarranted. They may feel responsible for the trauma they endured, leading to self-blame and a diminished sense of self-worth. This pervasive sense of shame can be emotionally crippling and prevent individuals from seeking help.
3. Hypervigilance
Hypervigilance is another common symptom of C-PTSD. Individuals may feel constantly on edge, always scanning their environment for potential threats. This heightened state of awareness can lead to chronic anxiety, sleep disturbances, and an inability to relax, as the brain is in a continuous state of alertness.
4. Flashbacks and Intrusive Thoughts
Like PTSD, individuals with C-PTSD frequently experience flashbacks and intrusive thoughts related to their traumatic experiences. These can occur unexpectedly and cause intense emotional distress, often making the individual feel as though they are reliving the trauma. Flashbacks can significantly impair daily functioning and emotional well-being.
5. Difficulty Trusting Others
Trust issues are a hallmark symptom of C-PTSD. Prolonged trauma, particularly in the context of abusive relationships, can lead to a deep mistrust of others. Victims may struggle to form meaningful connections, fearing that others may harm or betray them. This can result in social isolation and strained relationships.
6. Negative Self-Perception
Individuals with C-PTSD often harbor a deeply negative self-image. They may view themselves as worthless, broken, or undeserving of love and support. This negative self-perception can exacerbate feelings of depression and hopelessness, making it difficult for individuals to seek treatment or engage in positive coping strategies.
7. Emotional Numbness
Emotional numbness is another symptom frequently observed in individuals with C-PTSD. To cope with overwhelming emotional pain, individuals may shut down emotionally, becoming detached from their feelings and surroundings. This emotional detachment can create difficulties in interpersonal relationships, as the individual may struggle to connect with others on an emotional level.
8. Avoidance Behaviors
Many people with C-PTSD engage in avoidance behaviors as a way to minimize exposure to reminders of their trauma. They may avoid certain places, people, or activities that trigger memories of their traumatic experiences. While avoidance may provide temporary relief, it can also limit the individual’s ability to lead a fulfilling life.
9. Chronic Feelings of Hopelessness
C-PTSD often leads to chronic feelings of hopelessness. Individuals may feel trapped in their trauma, believing that their situation will never improve. This sense of hopelessness can lead to feelings of despair and may contribute to suicidal thoughts or behaviors.
10. Somatic Symptoms
C-PTSD can manifest through somatic symptoms, or physical symptoms without a medical cause. Common somatic symptoms include headaches, gastrointestinal issues, chronic pain, and fatigue. These physical complaints are often the body’s way of expressing emotional distress, and they can further complicate the individual’s overall health.
11. Relationship Difficulties
People with C-PTSD often experience relationship difficulties. Their inability to trust others, combined with emotional dysregulation and avoidance behaviors, can strain relationships with family, friends, and romantic partners. These challenges may lead to feelings of loneliness and isolation, exacerbating the individual’s emotional distress.
12. Persistent Feelings of Emptiness
Feelings of emptiness are commonly reported by those with C-PTSD. This emotional void can leave individuals feeling disconnected from themselves and their surroundings. The persistent sense of emptiness can contribute to feelings of depression and a lack of purpose or direction in life.
13. Dissociation
Dissociation is a coping mechanism often used by individuals with C-PTSD. During moments of intense stress or when confronted with trauma reminders, individuals may feel disconnected from their thoughts, emotions, or physical body. This dissociative state can range from mild detachment to more severe episodes where the individual feels completely removed from reality.
14. Difficulty Concentrating
People with C-PTSD may experience difficulty concentrating and maintaining focus. The constant state of hypervigilance and emotional distress can make it hard to focus on tasks or retain information. This can affect work performance, academic success, and daily responsibilities.
15. Self-Destructive Behaviors
Self-destructive behaviors are a concerning symptom of C-PTSD. Individuals may engage in risky activities such as substance abuse, self-harm, or reckless behavior as a way to cope with their emotional pain. These behaviors are often a reflection of the individual’s deep-seated feelings of worthlessness and despair.
16. Difficulty Regulating Sleep
Sleep disturbances are common among individuals with C-PTSD. Insomnia, nightmares, and difficulty falling asleep are often reported. Nightmares, in particular, may center around the traumatic events, causing individuals to wake up in a state of distress. The lack of restful sleep can exacerbate other symptoms, such as irritability and difficulty concentrating.
17. Inability to Experience Joy
Lastly, individuals with C-PTSD may struggle to experience joy or pleasure in activities they once enjoyed. This symptom, often referred to as anhedonia, is closely linked to depression and can make it difficult for individuals to engage in hobbies, social events, or any activity that might normally bring happiness.
What is Complex Trauma (C-PTSD)?
Complex Post-Traumatic Stress Disorder (C-PTSD) is a psychological condition that develops in response to prolonged or repeated exposure to traumatic events, typically in situations where an individual feels trapped and unable to escape. Unlike PTSD, which can result from a single traumatic event, C-PTSD often arises from chronic trauma such as ongoing abuse, neglect, or captivity.
The term “complex trauma” refers to the cumulative emotional, psychological, and physical impact of these long-lasting traumatic experiences. Individuals with C-PTSD often endure trauma that involves a sense of loss of control, betrayal, or emotional manipulation, often inflicted by someone they trust, such as a caregiver or intimate partner.
Key aspects of C-PTSD include:
- Emotional Dysregulation – Difficulty managing intense emotions such as anger, sadness, or fear.
- Negative Self-Perception – Persistent feelings of shame, guilt, or worthlessness.
- Difficulty Trusting Others – Fear of forming close relationships due to past trauma.
- Flashbacks and Intrusive Thoughts – Reliving the traumatic experiences in disturbing memories or vivid flashbacks.
- Chronic Hypervigilance – A constant state of alertness or fear of danger, even in safe environments.
C-PTSD can affect various aspects of an individual’s life, including emotional well-being, relationships, and day-to-day functioning. Healing from complex trauma often requires long-term, trauma-informed therapy, where individuals can process their experiences and develop healthier coping mechanisms.
What is Complex Trauma in Adults?
Complex trauma in adults is a profound psychological condition that arises from repeated exposure to traumatic events, often during childhood or over extended periods. Unlike single-event traumas, such as accidents or natural disasters, complex trauma is typically relational, occurring within relationships marked by control, power imbalance, and emotional or physical abuse. These events often occur during critical developmental stages, leaving lasting scars on a person’s emotional, cognitive, and social functioning.
Understanding Complex Trauma: An In-Depth Overview
Complex trauma refers to the chronic and repeated exposure to traumatic events, particularly during childhood. This can include physical, emotional, or sexual abuse, neglect, or domestic violence. Adults with complex trauma often experience difficulties in regulating their emotions, forming healthy relationships, and maintaining a positive self-image.
This type of trauma is sometimes referred to as developmental trauma, as it often occurs in early childhood when the brain and body are still developing. The sustained nature of the trauma has far-reaching impacts on how individuals view themselves and the world around them.
Symptoms of Complex Trauma in Adults
Individuals suffering from complex trauma exhibit a wide array of symptoms, many of which overlap with post-traumatic stress disorder (PTSD). However, complex trauma has distinct characteristics due to its repetitive nature. Key symptoms include:
- Emotional dysregulation: Adults with complex trauma often have intense emotions, such as anger, sadness, or fear, that they struggle to manage. These emotions can feel overwhelming and disproportionate to the situations that trigger them.
- Negative self-perception: Many adults with complex trauma develop deeply ingrained feelings of worthlessness, shame, or guilt. These feelings are often accompanied by a persistent belief that they are fundamentally flawed or undeserving of love.
- Difficulty with relationships: Due to trust issues, individuals with complex trauma may find it challenging to form or maintain close relationships. They may avoid intimacy altogether or, conversely, become overly dependent on others.
- Dissociation: This coping mechanism allows individuals to detach themselves from their traumatic experiences. Dissociation can manifest as feeling disconnected from reality or one’s own body and thoughts.
- Hypervigilance: Those with complex trauma are often in a heightened state of alertness, constantly scanning their environment for potential threats. This can lead to chronic stress, anxiety, and fatigue.
Causes of Complex Trauma in Adults
Complex trauma is often rooted in childhood experiences, particularly when a caregiver or trusted individual perpetrates the abuse or neglect. Key causes of complex trauma include:
- Childhood abuse: Physical, emotional, or sexual abuse during childhood is a leading cause of complex trauma. The betrayal of trust by a caregiver or authority figure leaves deep emotional scars that persist into adulthood.
- Neglect: Lack of care, attention, or basic needs during childhood can be just as harmful as direct abuse. Neglected children may feel invisible, unworthy, or abandoned, leading to a distorted self-image and relationship difficulties later in life.
- Domestic violence: Growing up in a household where domestic violence is prevalent can have long-lasting effects on a child’s sense of safety and security. Witnessing violence between caregivers can instill fear, anxiety, and emotional turmoil that persists into adulthood.
- Repeated medical trauma: Adults who experienced prolonged medical treatments or invasive procedures as children may develop complex trauma. The helplessness and fear associated with repeated medical interventions can mirror the emotional impact of relational trauma.
Long-Term Effects of Complex Trauma on Adult Life
The effects of complex trauma do not disappear with time; rather, they tend to manifest throughout adulthood in various ways. Some long-term effects include:
- Chronic health problems: Adults with complex trauma are at an increased risk for a variety of physical health issues, including autoimmune disorders, heart disease, and gastrointestinal problems. The body’s prolonged exposure to stress hormones, such as cortisol, can take a toll on overall health.
- Mental health challenges: Depression, anxiety, and personality disorders are common among those with complex trauma. The intense emotional swings, self-destructive thoughts, and persistent feelings of emptiness often lead to debilitating mental health challenges that require long-term care and management.
- Substance abuse: Many adults turn to drugs or alcohol to numb the overwhelming emotions associated with complex trauma. This maladaptive coping mechanism often exacerbates the emotional and psychological damage caused by the trauma.
- Difficulty in relationships: Trust issues, emotional instability, and an inability to communicate effectively can strain personal relationships. Adults with complex trauma may struggle to maintain friendships, romantic partnerships, or even professional relationships due to unresolved trauma from their past.
- Self-harm and suicidal ideation: The overwhelming feelings of shame, guilt, and worthlessness can sometimes lead to self-harm or suicidal thoughts. Individuals with complex trauma may feel hopeless, believing that their pain is insurmountable.
How Complex Trauma Differs from PTSD
While both complex trauma and post-traumatic stress disorder (PTSD) share similar characteristics, the key distinction lies in the nature and duration of the traumatic experiences. PTSD is typically triggered by a single, identifiable event, such as a car accident or natural disaster, while complex trauma arises from repeated exposure to trauma over an extended period, often during childhood.
Furthermore, individuals with complex trauma are more likely to struggle with identity issues, emotional regulation, and relational difficulties than those with traditional PTSD. The chronic nature of complex trauma also means that recovery can be more complex and long-lasting.
Treatment Options for Complex Trauma in Adults
Treating complex trauma requires a multi-faceted approach that addresses both the emotional and physical components of the condition. Some effective treatment options include:
- Trauma-focused therapy: Cognitive-behavioral therapy (CBT) and eye movement desensitization and reprocessing (EMDR) are often used to help individuals process and integrate traumatic memories. These therapies focus on reducing the emotional intensity of traumatic memories and promoting healthier coping mechanisms.
- Somatic therapy: Since trauma is often stored in the body, somatic therapies, such as yoga, mindfulness, or sensorimotor psychotherapy, can help individuals reconnect with their bodies and release pent-up tension or trauma stored in their muscles and nervous system.
- Group therapy: Sharing experiences with others who have endured similar trauma can be incredibly healing. Group therapy provides a supportive environment where individuals can learn from each other, build connections, and develop new coping strategies.
- Medication: In some cases, medication may be necessary to manage the intense emotional swings and mental health challenges associated with complex trauma. Antidepressants, anti-anxiety medications, or mood stabilizers can help reduce symptoms, though they are often used in conjunction with therapy.
The Road to Recovery
Recovery from complex trauma is a long and often challenging process, but it is possible with the right support and treatment. Healing begins by acknowledging the trauma and seeking professional help. It involves relearning how to trust, regulate emotions, and build healthy relationships. With patience, self-compassion, and professional guidance, individuals can reclaim their lives from the grip of trauma.